About Retinal Tear & Detachment
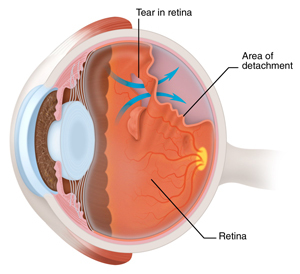
Retinal tear and retinal detachment are part of the same spectrum of disease requiring urgent, and frequently emergent, evaluation and treatment. In the young eye, the vitreous gel is in direct contact with the retina, the specialized, multilayered nerve tissue which lines the back of the eye. As the eye ages, the vitreous will shrink and separate from the retina. Most of the time the vitreous will separate cleanly without complication, but the patient may notice flashes and/or floaters. More rarely, the vitreous will remain attached to a part of the retina resulting in the development of one or more tears as the vitreous tries to pull away. If the retinal tear remains unrecognized and untreated, then fluid can rapidly accumulate through a defect (or multiple retinal defects). As the fluid builds up underneath the retina, retinal detachment, a blinding condition, can occur.
These conditions tend to be more common in near-sighted individuals, especially those with higher refractive errors (who need stronger spectacles or contact lenses). Others are born with a tendency to develop peripheral patches of thinning called lattice degeneration. Within these patches of thinning, multiple holes may develop spontaneously allowing fluid to accumulate leading to retinal detachment. This mechanism, or cause, of retinal detachment can be seen especially in younger patients before the vitreous gel separates. The vitreous tends to be more stuck to the retina around patches of lattice degeneration making an individual more vulnerable to developing retinal tear or retinal detachment during or following recent vitreous separation.
Symptoms
The symptoms of vitreous separation, retinal tear, and retinal detachment are similar and sometimes can overlap. On occasion, the patient may notice the floaters and flashing lights (photopsia) more commonly associated with isolated vitreous separation. The ophthalmologist, optometrist, or primary care physician should be suspicious about a more serious problem if the above symptoms are of very recent or sudden onset and are accompanied by a shower of spots or “cobwebs.” Of even greater concern is the loss of peripheral vision which may present as a shadow moving toward the center of one’s field of vision. These symptoms should prompt urgent evaluation and treatment as clinically indicated.
Diagnosis
Retinal tear and retinal detachment can be recognized during ophthalmoscopy, an examination performed by using a specially designed scope and magnified condensing lens, which allows a clear, three-dimensional, panoramic view of the peripheral retina. Another technique, used during ophthalmoscopy, involves gentle indentation of the eye wall with a blunt instrument to enhance the view of the peripheral retina. This technique can bring all abnormalities, which may require treatment, into view. This latter technique is more commonly and typically performed by the treating retinal surgeon who has been trained specifically to evaluate and manage these disorders. Sometimes a magnifying contact lens will be used during ophthalmoscopy to bring other details, not easily seen with indentation, into view. In rarer circumstances, the view of the retina itself may be blocked by the presence of blood in the vitreous called vitreous hemorrhage. In this situation, an ultrasound of the eye may be necessary to create an image from sound waves in order to make the diagnosis of retinal tear or detachment.
Treatment
If performed in a timely fashion, treatment of a retinal tear can prevent progression to retinal detachment. This treatment is accomplished by delivering either laser or cryotherapy (freezing technique) and is highly successful. The application of either of these techniques creates a scar around the retinal defect preventing the extension of fluid which could lead to retinal detachment.
Retinal detachment management depends on the degree of retinal involvement and symptoms the patient experiences. Many of these treatments can be performed in the office setting without the need for admission to a hospital or surgery center. Such treatment could involve laser (specially focused light) to block extension of a small, localized retinal detachment without any symptoms. Some retinal surgeons also use pneumatic retinopexy, which involves injecting a small gas bubble into the back of the eye. In a short period of time, this bubble can expand and close the retinal tear allowing the fluid under the retina to absorb. Following this treatment, the patient should be counseled to properly position his head in order to move the bubble over the tear. The tear can be treated either with laser or cryotherapy when the retina flattens.
More extensive retinal detachments will require surgical procedures such as scleral buckle or pars plana vitrectomy, which are performed in the operating room. A scleral buckle is a strip made of clear hard rubber which can be fastened to the eye wall in various positions to indent the eye permanently. This hardware gives the retina good peripheral support to promote healing of the detachment. Another increasingly used technique is pars plana vitrectomy, a surgical procedure which involves inserting specially designed small instruments into the eye to remove the vitreous gel which is pulling on the retina. This procedure usually is accompanied by injection of a gas bubble and laser therapy. As with pneumatic retinopexy, postoperative head positioning is required.
Complex retinal detachments may require a combination of vitrectomy and scleral buckle. In some chronic cases, scar tissue membrane sheets grow along the retinal surface and must be removed by a technique called membranectomy or membrane peel for the retina to successfully reattach.
Please call our office at 301.571.2000 to learn more about retinal tear and detachment or click here to schedule an appointment.