About Retinal Vascular Occlusive Disease
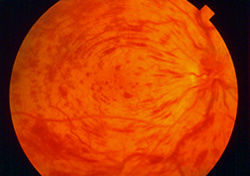
The retina is a thin sheet of nerve tissue in the back of the eye where light rays are focused and transmitted to the brain. Tiny blood vessels supply the retina with oxygen and other nutrients. Arteries deliver the blood, and the retinal veins carry it out. Sometimes one of these arteries hardens and presses on a nearby vein. The vein can then become blocked, or occluded, making it difficult for blood to leave the eye. This is called a retinal vein occlusion (RVO). A milder, less advanced form of this condition is also known as venous stasis retinopathy. The blocked circulation can lead to swelling and bleeding within the retina, growth of abnormal retinal blood vessels, and partial or total vision loss.
Retinal vein occlusions are the second most common cause of blood vessel-related vision loss (the first is diabetic retinopathy). The condition occurs most often in men and women over the age of 50, particularly those in their 60s and 70s. Risk factors include high blood pressure, high cholesterol, diabetes, smoking, glaucoma, and rarely, blood clotting and inflammatory conditions.
Treatment depends on the severity of the blockage and the location of the blocked vein. If the large central vein leaving the eye is affected, the condition is known as a central retinal vein occlusion or CRVO; otherwise it is called a branch retinal vein occlusion, or BRVO. BRVOs often can occur with no pain or noticeable loss of vision. It is important to have routine eye exams to detect any developing problems early. Patients can monitor their vision between appointments by closing one eye at a time.
Retinal vein occlusions are detected during a dilated retinal exam. A fluorescein angiogram may be performed to confirm the diagnosis and/or aid in treatment planning. Swelling of the macula, or macular edema, can be monitored using Ocular Coherence Tomography (OCT), a special type of retinal scan. Indications of an occlusion are bleeding in the eye, macular swelling or ischemia (loss of blood supply), and neovascularization – abnormal growth of new blood vessels. The retinal neovascularization can cause bleeding in the vitreous gel (vitreous hemorrhage) which can lead to severe vision loss if the blood does not clear on its own.
While there is no cure for retinal vein occlusions, patients are counseled to control high blood pressure, high cholesterol, diabetes and other health conditions that increase the risk of vascular hardening, narrowing and blood clotting.
Branch Retinal Vein Occlusions (BRVO)
Macular swelling used to be commonly treated with a light focal or grid laser, but more recently, intraocular injections of steroid (Triamcinolone), bevacizumab (Avastin),or ranibizumab (Lucentis)are now effective and more commonly used to treat macular edema, especially when the center of the macula, or fovea, is involved. When more of the retinal blood supply is damaged, this ischemia can cause abnormal blood vessel growth leading to vitreous hemorrhage.

Well-designed studies have shown that if this ischemic retinal damage is detected by careful examination and monitoring, scatter (or panretinal) laser treatment to the damaged area of retina can reduce or prevent vision loss. Even if new blood vessels are found before a serious bleed, such laser treatment is still helpful and may prevent the need for surgery to remove blood from the eye. If bleeding continues, a vitrectomy may be performed to remove the blood and its associated scar tissue if present. Scatter laser treatment also is performed at the time of surgery. Patients with a BRVO causing persistent visual problems may undergo a vitrectomy with an arteriovenous sheathotomy, a newer procedure in which the blocked vein is surgically separated from the artery compressing it. This procedure is not performed often since patients now can be stabilized or improved by the injection medicines introduced recently.
Central Retinal Vein Occlusions (CRVO)
Vision loss from CRVO most commonly is due to swelling of the central retina called macular edema. Unlike BRVO, grid laser treatment hasn’t been shown to stabilize or improve vision for CRVO. Recent studies have established that steroid or ranibizumab (Lucentis) injections in the eye can help patients with this disease.
As with other retinal diseases, bevacizumab (Avastin) is commonly used by retinal surgeons with varying degrees of success depending on advancement of disease. Avastin, Lucentis, and Eylea target Vascular Endothelial Growth Factor or VEGF, and limit the leakage of fluid out of the damaged blood vessels causing macular edema while steroids treat inflammation which also causes more macular edema. Long-term follow-up and treatment may be required to maintain vision. Ozurdex, an intravitreal sustained-delivery dexamethasone(steroid) implant is also an effective treatment for selected patients.
More advanced damage can lead to loss of retinal blood supply called ischemia. Large areas of ischemia can lead to abnormal blood vessel growth over the iris (colored part of the eye) leading to neovascular glaucoma, a very painful, blinding condition resulting from high pressure in the eye. Scatter (panretinal) laser, when applied to damaged peripheral retina, can make these abnormal blood vessels disappear if the treatment is performed in a timely fashion. Newer peripheral imaging techniques have shown that this periperhal ischemia may be present more often than previously recognized. Further research will help define new treatment approaches to prevent the sight-threatening complications of this disease.
Please call our office at 301.571.2000 to learn more about retinal vascular occlusive disease or click here to schedule an appointment.