Macular Hole
A macular hole is exactly what it sounds like: a hole in the macula, the center of the retina responsible for central and reading vision. This hole or defect occurs in the fovea, the center of the macula, and the most sensitive part of the entire retina.
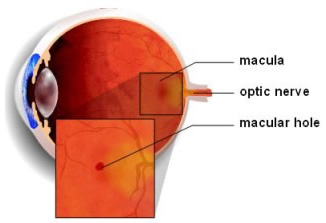
Macular holes most commonly develop spontaneously during the natural aging process, when the vitreous (the gel that fills most of the eye) becomes more like a watery liquid and separates from the retina. Rather than separating cleanly, the vitreous may abnormally stick to and pull on the macula causing a hole to form. Less commonly, macular holes are caused by direct, blunt eye injury or can occur with intraocular inflammation, macular pucker, or retinal detachment. Most cases occur in people over the age of 60.
At first, a macular hole may only cause a small blurry or distorted area in the center of vision. As the hole grows over several weeks or months, central vision progressively worsens. Peripheral vision usually is not affected, although in very rare instances such holes can cause retinal detachment. There are four stages of a macular hole: small foveal detachments with a partial-thickness defect (stage 1), small full-thickness holes (stage 2), larger full-thickness holes without vitreous separation from the retina (stage 3), and larger full-thickness holes with vitreous separation (stage 4). Each stage can progress to the next if not treated.
Macular holes can be closed surgically and successfully treated in approximately 90-95% of cases. The level of vision improvement and final result depend on the size of the hole, duration of symptoms, and the level of vision loss before surgery is performed. Typically, smaller macular holes with a short duration of symptoms and limited vision loss have the best results with treatment. The surgery involves vitrectomy, or separation and removal of the vitreous gel from the eye with injection of a gas bubble within the eye. This procedure is performed in the outpatient setting under local anesthesia either in a surgery center or hospital. After surgery, patients must position themselves face down, as instructed by the surgeon, to allow the hole to heal completely. As the eye heals, the fluid in the eye is naturally replaced.
A non-surgical alternative to treat macular holes is under development and investigation and awaits potential approval by the Food and Drug Administration (FDA). Ocriplasmin is a specially designed medicine injected in the eye which experimentally can dissolve the attachments of the vitreous gel to the retina. Recent studies have shown encouraging results and suggest that possibly 40% of holes may benefit without surgical treatment. Additional study is necessary to understand if this medicine will help the surgical treatment of macular holes.
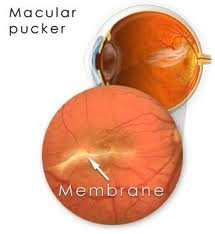
Macular Pucker
An epiretinal membrane, also called macular pucker, is a thin layer or sheet of scar tissue that forms and grows over the macula, the area of the retina that gives us clear central and reading vision.
Idiopathic or primary epiretinal membranes often develop on their own as a part of the natural aging process. These sheets of scar tissue most commonly grow after age-related vitreous separation. Less commonly with partial vitreous separation, tugging of the vitreous on the macula also can cause these membranes to form.
Epiretinal membranes also may result from eye conditions or diseases such as diabetic retinopathy, retinal detachment, inflammation, eye trauma, or retinal vein blockage. These are called secondary epiretinal membranes.
Many epiretinal membranes do not affect vision. Thicker membranes, however, can create a wrinkle or pucker of the macula as they grow over the surface of the retina. The retina can swell leading to macular edema. As this occurs, small blurry or distorted areas in the center of vision may develop. The growth of scar tissue can result in more visual distortion, blurring vision, and lead to severe central vision loss. Peripheral vision typically is not affected.
While many epiretinal membranes don’t progress enough to require treatment, surgery is recommended for those patients who experience troublesome vision loss. Surgery involves vitrectomy to remove the vitreous gel and membrane stripping to delicately peel the sheet of scar tissue away from the macular surface using tiny, specially designed instruments. The surgery is performed as an outpatient procedure with local anesthesia. There is no non-surgical alternative to treat epiretinal membranes at this time.
Please call our office at 301.571.2000 to learn more about macular hole / macular pucker or click here to schedule an appointment.