About Diabetic Retinopathy
Diabetes mellitus causes a persistent elevation of blood sugar which eventually results in damage to the blood vessels within the retina. These damaging changes are known as diabetic retinopathy.
Non-Proliferative Diabetic Retinopathy
Non-Proliferative Diabetic Retinopathy or NPDR is an early stage of disease where tiny red spots appear in the retina. These spots may represent blood (hemorrhage) or abnormal pouching of the tiniest blood vessels or capillaries (microaneurysms). The lining of these blood vessels can become damaged enough to allow leakage of fluid (serum) and/or fatty material (exudates) into the retina to cause swelling (edema). This swelling, if it involves the central retina, is referred to as macular edema.
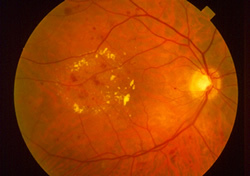
Such involvement of the macula can affect our high-resolution visual activities such as reading, driving, or threading a needle. As NPDR progresses, the smallest blood vessels (capillaries) can close leading to a loss of blood supply to the retina called ischemia.
Proliferative Diabetic Retinopathy
With more extensive loss of blood supply and because the retina is so oxygen-needy, abnormal new blood vessels (retinal neovascularization) will grow in an effort to supply blood to damaged retina. This more advanced stage of disease, called Proliferative Diabetic Retinopathy or PDR, can lead to severe vision loss if not recognized and left untreated. The abnormal new blood vessels typical of PDR do not resupply the retina and are extremely fragile unlike normal healthy retinal blood vessels. As the abnormal blood vessels grow along the surface of the retina, optic nerve, and into the vitreous cavity (the clear jelly-like sac which occupies the center of the eye), bleeding (vitreous hemorrhage) can occur. If the hemorrhage is small, the patient may only notice spots, floaters, or “cobwebs.” Larger hemorrhages can lead to severe loss of central and peripheral vision.
With advancement of disease, scar tissue can grow with the abnormal new blood vessels. As the scar tissue contracts, it can pull on the retina resulting in traction retinal detachment. Limited involvement of the macula may result only in visual distortion, but larger areas of detachment can result in severe vision loss. Sometimes the retinal ischemia can be so extensive that abnormal blood vessels will grow over the iris which is the colored part of the eye. If this occurs, the new blood vessels can scar the front of the eye and block normal outflow of fluid resulting in a frequently painful and potentially blinding condition called neovascular glaucoma.
Treatment
Landmark clinical trials have established that careful and strict control of blood sugar will significantly reduce one’s risk of vision loss from diabetic retinopathy. Even in patients who have evidence of retinopathy, improving blood sugar control can lower the risk for long-term progression of disease.
Laser. Laser treatment (specially focused light), has been the established standard-of-care for diabetic retinopathy for decades. A small focal or grid laser treatment can be applied to treat macular edema by reducing leakage from the damaged blood vessels near the macula. This treatment has been shown to limit worsening of edema and the risk of further vision loss. Panretinal Photocoagulation or scatter laser treatment is used to manage the abnormal new blood vessel growth from PDR. The peripheral damaged retinal tissue is treated so that the new blood vessels will shrink and limit or prevent additional scar tissue growth which could lead to vitreous hemorrhage and retinal detachment. It’s not uncommon for both types of laser treatment to be repeated as necessary to stabilize but not cure the disease.
Intravitreal Injections
During the past decade intravitreal steroids and bevacizumab (Avastin) have been used in an “off-label” fashion as additional treatments for diabetic retinopathy. These medicines, when injected into the eye, can control inflammation and Vascular Endothelial Growth Factor (VEGF) expression, both of which have been shown to cause retinopathy progression, in the eye. Ranibizumab (Lucentis) also targets VEGF and has very recently received approval for treatment of diabetic retinopathy. Aflibercept (Eylea) is another FDA-approved agent which is similarly effective to other anti-VEGF agents and in some patients with poor vision may represent a more advantageous treatment functionally. Ozurdex is an FDA-approved sustained-release intravitreal steroid implant that is very effective in treating diabetic macular edema (DME) and has the advantage of exerting a more durable treatment effect allowing a reduction in frequency of eye injections. As with other steroid preparations used in and around the eye, there is an increased risk of cataract progression and glaucoma.
Vitrectomy
With advanced disease (PDR), non-clearing vitreous hemorrhage and retinal detachment can lead to severe vision loss. Pars Plana Vitrectomy is a surgical procedure using tiny instruments to mechanically remove the vitreous gel and abnormal blood contained within it. Additional scatter laser treatment can also be performed within the eye during surgery. Scar tissue causing retinal detachment or macular pucker is also removed. The clearing of vitreous hemorrhage and repair of retinal detachment can stabilize and improve vision.
Please call our office at 301.571.2000 to learn more about diabetic retinopathy or click here to schedule an appointment.